Nurses need physiology biliary obstruction and pancreatitis – Nurses play a pivotal role in the management of biliary obstruction and pancreatitis, two prevalent conditions with significant implications for patient outcomes. Understanding the physiology of these conditions is essential for nurses to provide effective and compassionate care. This article delves into the physiological processes underlying biliary obstruction and pancreatitis, highlighting the impact on nursing practice and the importance of interdisciplinary collaboration.
The physiological mechanisms leading to biliary obstruction and pancreatitis are complex, involving anatomical structures such as the biliary tree and pancreas. Nurses must grasp these mechanisms to assess and intervene appropriately. Hormonal and neural pathways also influence the development and progression of these conditions, necessitating a comprehensive understanding of their role.
Physiology of Biliary Obstruction and Pancreatitis
Biliary obstruction and pancreatitis are conditions that can significantly impact the gastrointestinal system. Understanding the physiology behind these conditions is essential for effective nursing care.
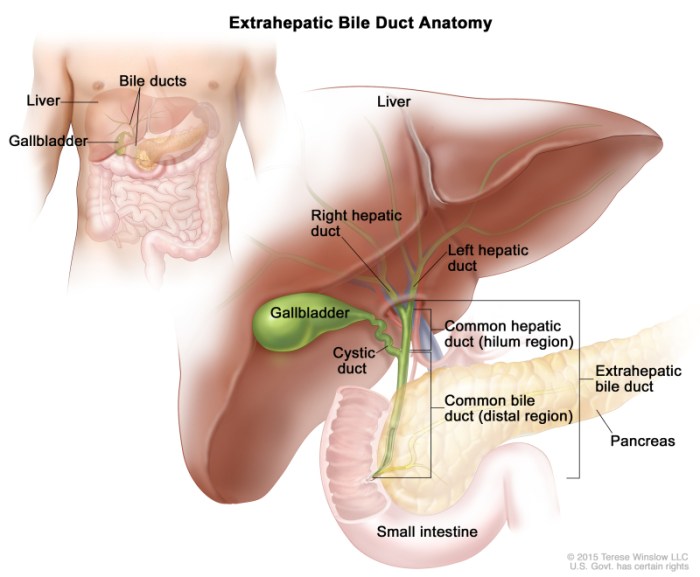
Anatomical Structures Involved, Nurses need physiology biliary obstruction and pancreatitis
Biliary obstruction occurs when the flow of bile from the liver to the small intestine is blocked. The anatomical structures involved in biliary obstruction include:
- Liver
- Gallbladder
- Bile ducts
- Pancreas
- Sphincter of Oddi
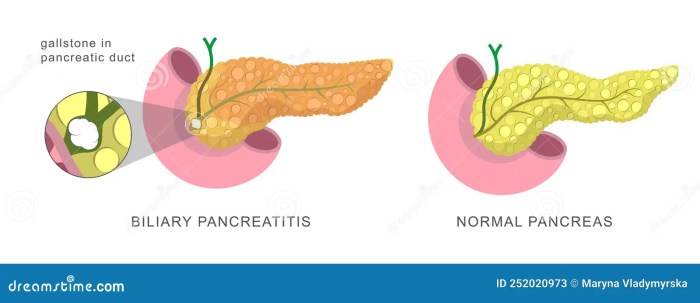
Pancreatitis is an inflammation of the pancreas. The pancreas is a gland located behind the stomach that produces enzymes and hormones involved in digestion and blood sugar regulation.
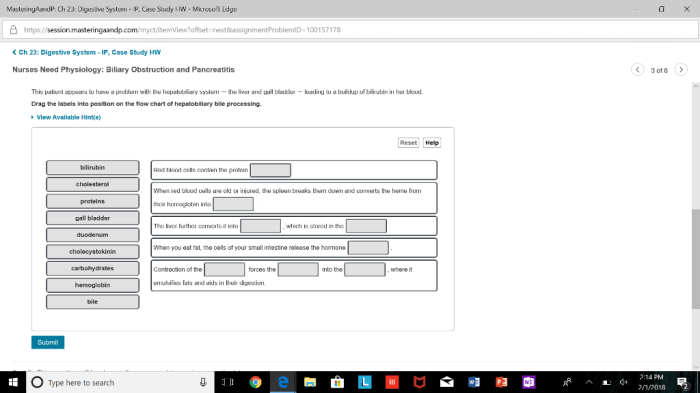
Physiological Processes
Biliary obstruction can result from factors such as gallstones, tumors, or inflammation. When bile flow is blocked, it can lead to the accumulation of bile in the liver and gallbladder, causing inflammation and pain. Pancreatitis can be caused by factors such as gallstones, alcohol abuse, or trauma.
Inflammation of the pancreas can lead to the release of enzymes that can damage the pancreas and surrounding tissues.
Hormonal and Neural Mechanisms
Hormonal and neural mechanisms play a role in biliary obstruction and pancreatitis. Cholecystokinin (CCK) is a hormone that stimulates the contraction of the gallbladder and relaxation of the sphincter of Oddi, allowing bile to flow into the small intestine. Other hormones, such as secretin and glucagon, also influence bile flow.
The vagus nerve and splanchnic nerves provide neural innervation to the biliary tract and pancreas, influencing their function.
Impact of Biliary Obstruction and Pancreatitis on Nurses
Biliary obstruction and pancreatitis can have a significant impact on nurses, as they are often responsible for assessing, monitoring, and managing patients with these conditions.
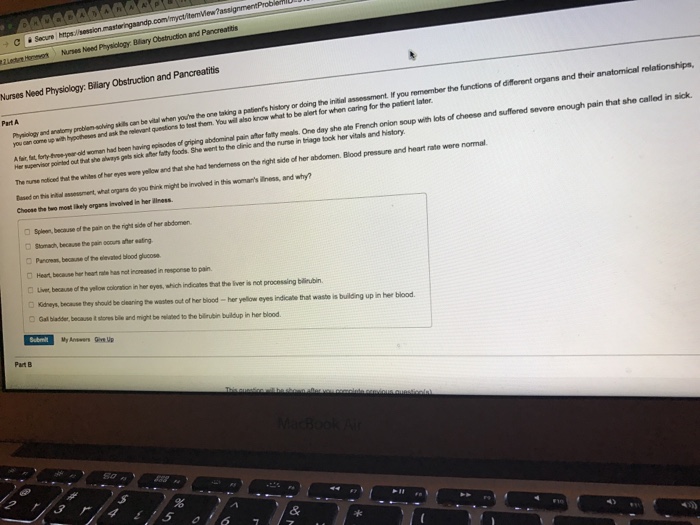
Nursing Assessments
Nursing assessments for patients with biliary obstruction and pancreatitis include:
- Medical history and physical examination
- Pain assessment
- Vital signs
- Abdominal examination
- Laboratory tests (e.g., liver function tests, pancreatic enzymes)
- Imaging studies (e.g., ultrasound, CT scan)
Nursing Interventions
Nursing interventions for patients with biliary obstruction and pancreatitis include:
- Pain management
- Nausea and vomiting management
- Nutritional support
- Hydration
- Monitoring for complications
Pain Management
Pain is a common symptom of biliary obstruction and pancreatitis. Nurses play a crucial role in assessing and managing pain using various interventions, including:
- Pharmacological interventions (e.g., opioids, nonsteroidal anti-inflammatory drugs)
- Non-pharmacological interventions (e.g., heat or cold therapy, massage)
Nursing Care Plan for Biliary Obstruction and Pancreatitis
A comprehensive nursing care plan is essential for effective management of patients with biliary obstruction and pancreatitis.
Nursing Diagnoses
Common nursing diagnoses for patients with biliary obstruction and pancreatitis include:
- Acute pain
- Nausea
- Vomiting
- Imbalanced nutrition: Less than body requirements
- Fluid volume deficit
Goals
Goals for nursing care include:
- Relief of pain
- Control of nausea and vomiting
- Maintenance of adequate nutrition
- Maintenance of fluid balance
- Prevention of complications
Interventions
Nursing interventions for each nursing diagnosis should be evidence-based and tailored to the individual patient’s needs.
Evaluations
Regular evaluations are essential to assess the effectiveness of nursing interventions and make necessary adjustments to the care plan.
Interdisciplinary Collaboration in Managing Biliary Obstruction and Pancreatitis
Effective management of biliary obstruction and pancreatitis requires collaboration among various healthcare professionals.
Roles of Healthcare Professionals
Healthcare professionals involved in the care of patients with biliary obstruction and pancreatitis include:
- Nurses
- Physicians (e.g., gastroenterologists, surgeons)
- Dietitians
- Pharmacists
- Social workers
Communication and Coordination
Clear communication and coordination among healthcare professionals are crucial to ensure continuity of care and prevent errors. Effective strategies include:
- Regular interdisciplinary meetings
- Use of electronic medical records
- Establishment of clear roles and responsibilities
Patient Education and Support for Biliary Obstruction and Pancreatitis: Nurses Need Physiology Biliary Obstruction And Pancreatitis
Patient education and support are vital for successful management of biliary obstruction and pancreatitis.
Patient Education Materials
Patient education materials should include information on:
- Causes and symptoms of biliary obstruction and pancreatitis
- Treatment options
- Lifestyle modifications
- Self-management strategies
Emotional Support
Patients with biliary obstruction and pancreatitis may experience emotional distress. Nurses play a crucial role in providing emotional support and counseling, including:
- Active listening
- Empathy
- Referral to support groups or mental health professionals
Clarifying Questions
What is the primary role of nurses in managing biliary obstruction and pancreatitis?
Nurses are responsible for assessing patients, implementing interventions, monitoring outcomes, and providing education and support to patients and their families.
How do nurses manage pain associated with biliary obstruction and pancreatitis?
Nurses administer pain medication, employ non-pharmacological pain management techniques, and collaborate with other healthcare professionals to optimize pain control.
What are the nutritional considerations for patients with biliary obstruction and pancreatitis?
Nurses ensure adequate nutritional intake through enteral or parenteral nutrition, monitor for complications, and provide dietary counseling.